In the Nordics, we are closer than most other countries to having one common health record for our citizens. Yet, when it comes to collaborating across sectors, we face big challenges.
In the center, the traditional healthcare delivery model in the Nordics has had the large, academic medical centers (AMCs) providing both general and specialized care. Community medical centers provide general care and feed patients that require advanced care to the AMCs. In addition, primary care physicians and municipalities play an important role, while the private sector has played a very modest role. Healthcare is largely government funded and there was limited choice – you went to the hospital where you lived. However, times are changing. Today, we see more and more patients choosing where they go for care. They may go to the hospital in the neighboring town or even leave their home country to skip waiting lines or to seek out better care. In the Nordics, private care is growing and the new public hospitals being built are smaller than the ones they are replacing. New treatments and guidelines are allowing for shorter hospital lengths of stay, thus decreasing the needs for hospital beds, while increasing the demands on staff and technology for the patients that remain as the only patients that remain in aggregate are sicker than in years past.
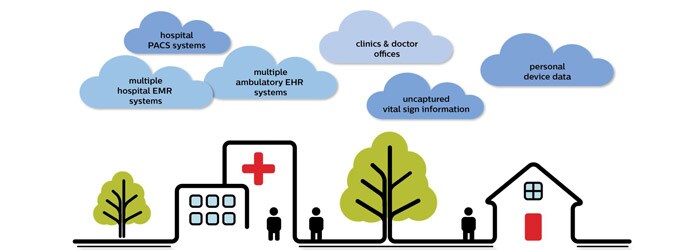
However, despite this progress, seemingly simple tasks are made challenging due to a concept some refer to as DRIP, we are Data Rich, but Information Poor. A phenomenon that is prevalent when the level of integration is low. Where reports or interfaces are not readily available on the same platform, it could take weeks of manual labor to gather the appropriate data when it could have taken days or even hours. At present, hospitals are required to use several different systems to gather information on the same patient. Future Health Index Philips recently commissioned a health study, the Future Health Index, that looks at access to care, integration of care and the implementation of connected care technologies. The results found that generally, there is high interest among caregivers and patients for the technology because they believe that it will bring value. However, what was surprising was that Sweden (the only Nordic country represented in the study) saw a huge disconnect between the investments being made and the value the technologies provided. Unfortunately, this is largely the case across all the Nordic countries. Bridging the gap Those with experience working in healthcare are probably familiar with innovation and brainstorming sessions where the goal is to develop new solutions for patients. Often a stakeholder map is created, here patients are put in the middle and the caregivers are placed around the patient. However, when looking at it from a business perspective and considering whom the technology is being sold to, technology vendors start to think about the hospitals and end up developing solutions the industry think they need rather than what the patients need. It is time to remember who is ultimately consuming healthcare services. We need to remember that the patient is the only constant in the care continuum; they are the end user of the data. With rapid technological advances and standardization of interfaces, we now have the infrastructure to achieve more seamless care. Furthermore, with the implementation of GDPR (General Data Protection Regulation), we also have a catalyst and enabler that provides us with a framework to work in. Online shopping, online banking, etc. are all possible – why not make online health management possible, too?
At Philips, we see a future where consumers are the ones driving sustainable healthcare transformation. We see a future, that is here now, where the patient owns their health data and provides access to the caregivers depending on what they are seeking care for. By doing this for the health care system, we can change the entire way we provide care in the Nordic countries – data is available whenever wherever for the persons authorized to access it. But the only way we see this working is by having an open healthcare IT ecosystem. Only by having an open system where you can have multiple developers developing their apps and multiple vendors providing their technical solutions can you actually have a system that designs in privacy, empowers and provides control to the citizens, and is personally configured.
Dela på sociala medier
Ämnen
Författare

Egil Nilsen Principal, Philips Nordic Health Care Transformation Services Based in Copenhagen, Egil Nilsen leads Philips Healthcare Transformation Services (HTS) consulting in the Nordics. Focusing on performance improvement, digitalization and innovation, he provides strategy and operations advice to hospitals, health systems, private healthcare organizations and public authorities. He received a master of science in industrial engineering and a bachelor of science in mechanical engineering, both from the University of Wisconsin - Madison.













